As mentioned in Part 1 of this series, your body will learn to overcompensate for weakened, painful and tightened muscles. Over time, connective tissues (called fascia) form lines of strain along these contracted, tense muscles.
Think of fascia as a net that holds your muscles, tendons and skin together, but still elastic enough to allow for movement. Fascial bands are connected all around your body, so when lines of strain are present, this will impact other areas, like a domino effect. Fascial strains both tighten and stretch tissues (think of the tight back / weakened abdominals example in the previous post) and also affects nerves and blood vessels.
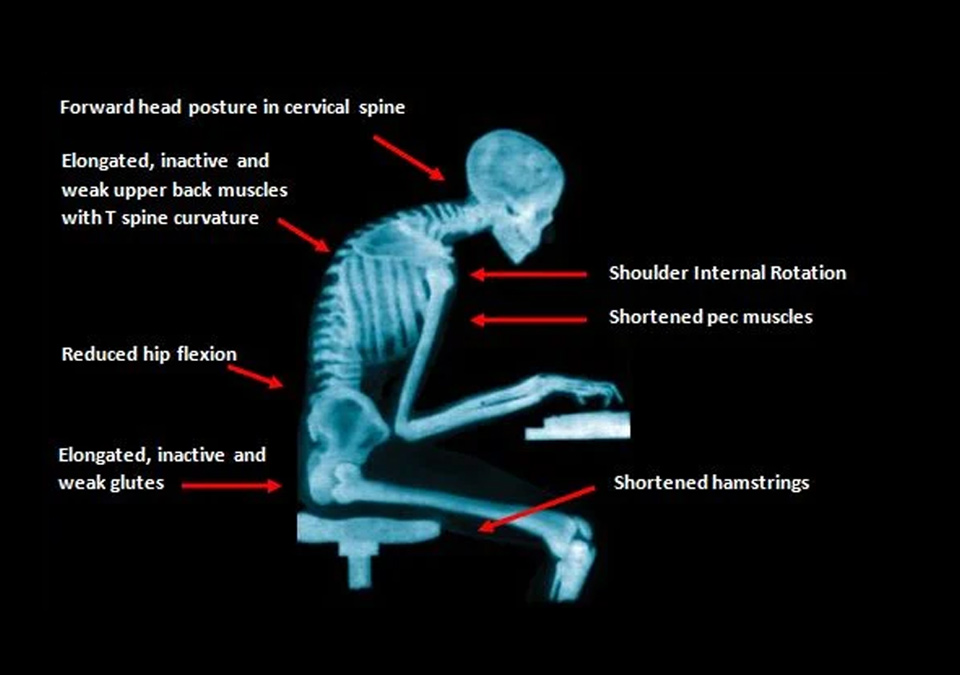
Eventually, new areas of the body will experience tension, toxin buildup, inadequate oxygen supply, inflammation and weakness. This leads to new types of compensation patterns, and the cycle begins all over again. What begins as a tight back and weak abdominals can progress into weakened glutes and overstretched hamstrings.
This ongoing cycle leads to complicated movement patterns that are harder to address as more muscles become involved. These muscles either become overactive or underactive, leading to further imbalances. When one muscle is too tight, its opposite can’t function optimally – again, think of the tight back and weakened abs.
As fascia and muscles contract more, the attachments between bones and tendons start to stretch. Tendons attach onto a lining over your bones, which is called a periosteum layer. When this layer gets stretched, it begins pulling away from the bone, and over time this becomes painful. This leads to periosteal (bone) pain.

To cope with chronically tense muscles and overly weak muscles, your body will produce new connective tissues around these areas for extra support. However, this doesn’t solve the problem. Instead, this leads to scar tissue buildup and joint restrictions, which can severely limit your range of motion and furthers muscular imbalances.
Ongoing imbalances and lack of treatment will eventually lead to full-body dysfunction, which will be further discussed in the next and final post of this three-part series, Setting the Tone.
